What will tomorrow’s world look like—a world that has implemented the innovations pioneered today? A world based on the groundbreaking technological, social, and political ideas that have only just surfaced? In this series, Metals Magazine’s independent editor James Gray takes a peek into his crystal ball and lets us know what the future holds and explores the world of telemedicine.
Let me introduce you to two very close friends of mine, Miki and his heavily pregnant wife, Ahnah. They are a young, fit, and adventurous couple, who live in the small town of Trapper Creek, population 423, some 117 miles by road from Alaska’s largest city of Anchorage. I befriended them a few years ago during a running retreat in British Columbia. These days, they are excited and scared in equal measure at the prospect of becoming first-time parents. Miki works in oil and gas extraction and spends long hours away from home, which makes it all but impossible for the couple to follow the traditional prenatal care route of upwards of 14 in-person visits throughout pregnancy. The pressures of significant travel time and time off work are simply too much.
Fortunately, Ahnah is in the care of a forward-thinking physician who recognizes that not all prenatal visits require in-person care—such as those for ultrasounds and lab tests—, and with Ahnah’s pregnancy classed as low-risk, her physician was quick to recommend telemedicine for almost half of her consultations. Miki and Ahnah are equipped to monitor blood pressure, weight, fetal heart rate, and other maternal and fetal vitals at home, which allows continuity of care to be ensured while enabling the future parents to contribute to their care plan from the convenience of their own home.
Bringing medical expertise to remote communities like Miki and Ahnah’s has obviously been life-changing—and there are plenty of small and often inaccessible populations throughout Arctic Alaska that do not even have a nurse practitioner, let alone a doctor, and where emergencies sometimes require a team of Huskies to transport patient records via sled. Out of necessity, Alaska became an early adopter of telemedicine as a solution to bridging the gap between patients and doctors, so telehealth services have already been available for more than two decades; the Alaska Native Tribal Health Consortium, for example, has been offering such services since 2001.
Any innovation in such a critical area as healthcare will take time to earn validation and gain traction, and telemedicine has been waiting to be embraced by the global medical community for years already. But there are many more factors in play than simply providing essential care to remote areas. Telemedicine has been threatening to transform the healthcare landscape for a while, and the coronavirus pandemic has unquestionably hastened its arrival. Hospitals overwhelmed with coronavirus patients have been forced to minimize the number of on-site medical procedures and postpone non-critical medical services, increasingly turning to telemedicine to maintain clinical services while also adhering to strict social distancing protocols.
With patients becoming accustomed to the level of acces telemedicine provides, I don’t think we’re ever going to be able to go back. The box is open.”
Dr. Jeffrey English
Neurologist
Telemedicine is sometimes used interchangeably with telehealth, although there is a difference in that telemedicine, as defined by the U.S. National Institutes of Health (NIH), is “the use of technology to provide and support healthcare at a distance,” while telehealth refers to a broader scope of remote healthcare services that also include remote non-clinical services such as provider training, administrative meetings, and continuing medical education. Telemedicine, therefore, allows doctors to diagnose and treat patients remotely using telecommunications technology. It is both convenient and cost-effective. It relies on technologies that cover the entire spectrum from telephones and text messaging to transmitted images and videoconferencing.

Slow adoption rates
Why has the medical community been so slow to adopt telemedicine? Doctors have always cited the main factor as the difficulty in being able to make an accurate assessment from a distance, given that a physical examination is impossible in telemedicine scenarios, where they are forced to rely on the patient’s own verbal description of their medical issue. During in-person visits, doctors are more sensitive to the visual clues that aid diagnosis. And the slow uptake has undoubtedly been compounded by the fact that many patients are not even aware of the availability of such an option.
Meanwhile the pandemic has reduced patients’ access to doctors and provided a catalyst for significantly increased use of telemedicine by healthcare systems worldwide, which is in stark contrast to previously slow adoption of this innovative practice. According to a study conducted in April 2020 by Sermo, a collaborative platform built specifically for physicians, 63% of healthcare professionals have used telemedicine to consult with patients since the outbreak of the pandemic, with an average 57% of patients treated via telemedicine globally at its height. This represents a significant uptake in the use of telemedicine; in February 2020, some 66% of patients were reported to have never previously consulted with a doctor via telemedicine.
If telemedicine continues along this trajectory—and as the swirling mists inside my crystal ball begin to clear, all the evidence suggests that it will—, it is likely to completely redefine how health systems are run, how they deliver care, and how costs are managed.
If there’s a silver lining to Covid-19, it’s the advances made in telehealth.”
Thomas Ely
President of the American Osteopathic Association
Post-pandemic uptake
While the coronavirus has unquestionably accelerated the adoption of telemedicine, it’s clear we have reached a tipping point from which there’s no going back. Prior to Covid-19, annual revenues of telehealth stakeholders in the U.S.A. were reported at around 3 billion dollars, a figure which experts believe could easily skyrocket to as much as 250 billion (for more on the uptake of telemedicine post-Covid-19 see “Telehealth: A quarter-trillion-dollar post-COVID-19 reality?“). So I fully expect telemedicine to become a standard service that will be offered across all healthcare scenarios.
What this also leads me to believe is that patients will become increasingly selective. It is very likely that patients will prioritize criteria such as access to telemedicine services in their choice of healthcare provider. After all, if you can reduce waiting times, enjoy greater convenience, and still expect equally high-quality care, why wouldn’t you go down the telemedicine route?
Equally, medical facilities prepared to embrace telemedicine can expect their revenues to grow exponentially. Telemedicine offers another revenue stream that can bridge the gap in the face of any future drop in patient numbers caused by unexpected events—such as a pandemic. According to the American Hospital Association, hospitals in the U.S.A. lost an estimated 202.6 billion dollars between March and June 2020 alone. So it makes perfect sense for any medical facility to add telemedicine to their arsenal. Dr. Tom Tuzel, a New York Psychiatrist, says, “Patients are now requesting telemedicine. We’ve seen volumes and business increase significantly this year because the competition was slower to adopt and offer telemedicine.”
Preventive care is another area that stands to benefit hugely from telemedicine. According to the Centers for Disease Control and Prevention (CDC), up to 75% of U.S. healthcare spending is accounted for by avoidable chronic diseases. Dr. Tom Tuzel goes on: “The goal of the future care is preventative and to make as many adjustments early on. How do you do that in a cost-effective, time-effective manner? With technology and telemedicine services.”
Store-and-forward
Data acquired from the patient such as medical images or biosignals is sent to the physician. This practice is popular in dermatology, radiology, and pathology.
Remote monitoring
Uses a range of technological devices to monitor a patient’s health from a distance. It is effective in the management of chronic diseases such as cardiovascular disease, diabetes mellitus, and asthma.
Real-time interactive services
Are effective in providing immediate advice. This can be done by phone or using videoconferencing tools. Examples include teleneuropsychology, telenursing, telepharmacy, and telerehabilitiation.

From evolution to revolution
The shift toward greater use of telemedicine has been slow—until now. But while progress has so far been gradual, the pandemic could be regarded as the straw that broke the camel’s back—and the eventual changes will be seismic. Make no mistake, it will require a change in mindset from both patients and doctors, the implementation and integration of new and groundbreaking technologies, and new ways of working. But every one of us is more than capable of adapting and learning. Just consider for a moment how many of us—however reluctantly at first, perhaps—have begun to take working from home in our stride and now use teleconferencing tools on an almost daily basis to communicate and collaborate.
It’s an exciting shift and the benefits are huge: greater convenience and easier access to high-quality healthcare will inevitably increase patient confidence and drive growth, leading to better patient outcomes and a more efficient and effective healthcare system. It’s an exciting time generally for the medical community: the European Patent Office recently reported that, despite the pandemic, innovation in healthcare was the main driver of European patent applications in 2020.
Telemedicine can without a doubt help to redress the balance in terms of disparities in the provision of care. For instance, the Inuit in Canada’s far north have lifespans 12 to 15 years shorter than the average Canadian’s, and telemedicine can help to bring much needed expertise to these remote populations so that they no longer have to rely on air transport to ensure access to specialists. In Alaska as well, telemedicine has the potential to balance out inequalities in care services between remote communities and more heavily populated urban areas. Which brings me neatly back to Trapper Creek, where, I think, Miki and Ahnah have every reason to be a lot more excited and a lot less scared about becoming parents. I, for one, have every confidence in their physician’s advice to embrace telemedicine, and I cannot wait for the birth of their healthy baby … daughter. Oops, have I given it away?
In the absence of any official definition, “Long Covid” refers to symptoms such as breathlessness, fatigue, or anxiety that are still felt three months after the original infection. It is said to affect roughly two thirds of patients hospitalized by Covid, and around 10 percent of those who suffered only mild symptoms.
In the U.K., a revolutionary remote-treatment initiative is now being rolled out in hospitals: the Living With Covid Recovery program. It is a treatment plan provided to patients at home from a distance using a tablet device or smartphone app. Because rehabilitation is delivered entirely remotely, it allows National Health Service (NHS) staff to support many more patients than would otherwise be possible. The trial that preceded rollout showed that 122 people could be processed in one morning by a single person, compared with just 15 patients a week for in-person visits.
Combining evidence-based methods from physiotherapists, psychologists, dieticians, and respiratory physicians, it allows personalized treatment plans to be created and delivered remotely via a dashboard that is used by an assigned nurse or therapist to track a patient’s health and progress, and to adapt treatment accordingly. Project leader Elizabeth Murray, a general practitioner and professor of e-health at University College London, says: “I’ve worked in digital health for 20 years and I’ve never seen anything get taken up so fast and so widely as this.” The team behind the program is talking to the World Health Organisation about a global rollout.

Cybersecurity: Telemedicine and Blockchain
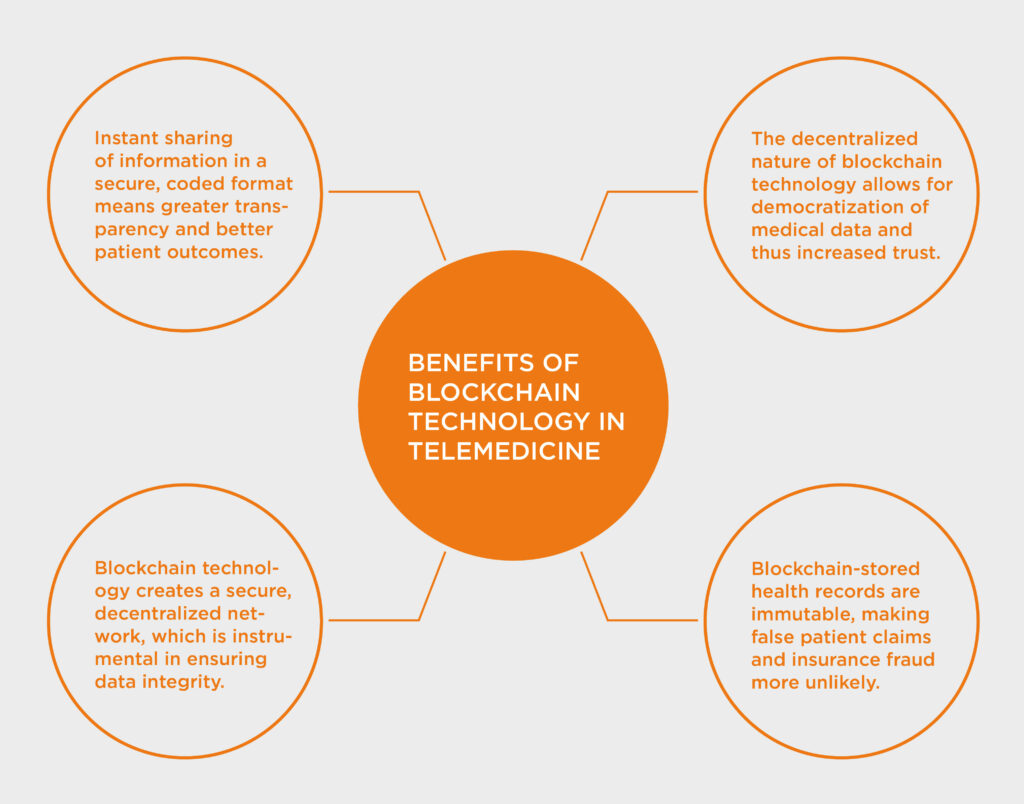
A blockchain is a digital record of transactions, a growing chain of time-stamped and immutable blocks that contain information. Essentially, it is a database—or digital ledger—that is shared across a network of computers not owned by any single entity. The technology allows digital information to be shared but not copied, making it difficult or even impossible to change or hack the information.
So where might blockchain technology fit in with telemedicine? Half of all healthcare organizations in the U.S.A., for instance, have already adopted telemedicine in some form, and with data security and privacy so crucial to patient data, especially in the context of what has been described as an increasingly “trustless society,” the advantage of blockchain technology lies in ensuring secure, immutable, and decentralized transactions. It is a sad truth that telemedicine is not a hundred percent immune to hacking, and because trust in telemedicine among patients and providers alike is at the very heart of telemedicine’s success, cybersecurity has to be made a top priority. Telemedicine platforms therefore have to be designed from the ground up to be bulletproof.